Fulminant hepatic failure induced by antipsychotic drugs (a case report)
Open Access Journal of Toxicology
Introduction
Fulminant hepatitis is a rare condition but has a very poor prognosis in the absence of liver transplantation. It is important to identify the cause as soon as possible to start the etiological treatment, which may be drug poisoning, viral hepatitis, or alcoholic ... [1-3]. N-acetylcysteine (NAC), a glutathione precursor, was first used as a treatment for paracetamol overdose in 1979. Since then, it has been firmly established as an effective and safe treatment for paracetamol induced IHC prevention. NAC has also been shown to be effective outside paracetamol intoxication. It has been evaluated as an option for acute IHC other than paracetamol in adults and children. In a randomized clinical trial comparing NAC with placebo in adults with paracetamol-free IHC, NAC was associated with a marked improvement in survival without liver transplantation [4]. NAC has also been evaluated for non-hepatic clinical conditions, these indications include its use in lung diseases (COPD and pulmonary fibrosis), in the prevention of contrast-induced nephrotoxicity and for the treatment of certain cardiac diseases [3,5]. In this article, we report the case of a neuroleptic overdose in a 16-year-old who has rapidly progressed to fulminant hepatitis. The oral administration of N-acetylcysteine has allowed a dramatic improvement [3].
Observation
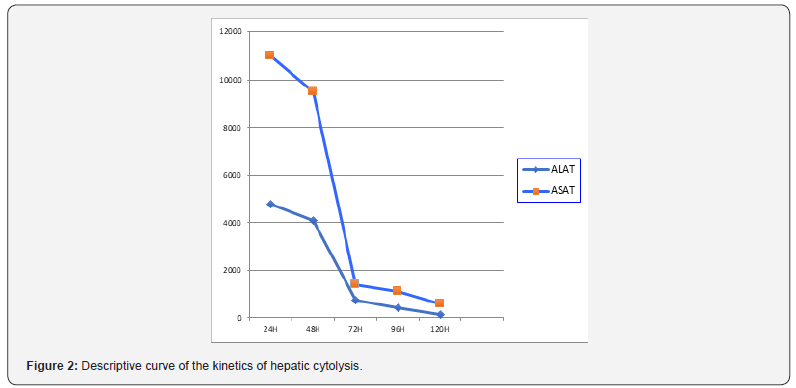
A 16-year-old man consulted at the emergency reception service (j1) for asthenia, disabling diffuse myalgia and uncontrollable vomiting, in the context of cutaneous-mucous jaundice, which had appeared for 4 days. Her antecedents included herpetic keratitis since the age of 3 years and chronic epigastralgia for 4 years. In the emergency department, the clinical examination found a sleepy, sleepy patient, a conjunctival subitem, muscle pain with manual pressure. The temperature was 37.8°C, and blood glucose was 2.2mmol/l. The blood pressure was 85/38 mmHg, the heart rate was 104 beats per minute and 95% saturation in the air. The biochemical assessment was very disturbed, with: an inflammatory syndrome (C-reactive protein at 150 mg/L, fibrinogen at 6.6g/L), renal insufficiency (urea at 14.4mmol/L, creatinine at 159 , 12mmol/L), cytolysis (ASAT: 10454 IU/L, ALA at 4408 IU/L), cholestasis (conjugated bilirubinemia at 151mmol/L, gamma GT at 489 IU / L, PAL at 657 IU/L ) and a disturbance of its hemostasis (TP <15%, a TCA at 96.4 s and a very collapsed factor V). The hemogram showed the following: white blood cells at 9210mm-3, platelets at 159 000mm-3 and hemoglobin at 11.2g/dl.
On the diagnosis side
The patient was admitted to intensive care (1st day). Etiologically, an infectious hypothesis has been ruled out by the negativity of his liver serologies (anti-HVA Ab, anti-HBV Ab and HBs antigen and anti-HCV antibodies) as well as the serology of CMV, the abdominal ultrasound was without particularities, blood ceruloplasmin level was normal, anti-smooth muscle and antimitochondrial antibodies were achieved returning normal. The preferred toxic hypothesis was a neuroleptic overdose because the interview reported a prescription of 3 different neuroleptics, by his doctor for his chronic epigastralgia of psychogenic origin (Olanzapine, Mainspring and Metoclopramide). Supported: Symptomatic treatment consisted of stopping neuroleptics, infusion of fresh frozen plasma, vitamin K, laxatives and ciprofloxacin were initiated associated with administration of N-acetylcysteine with a dose of oral load of 140mg/kg followed by a dose of 70mg/kg/day maintenance for 48 hours.
Evolution
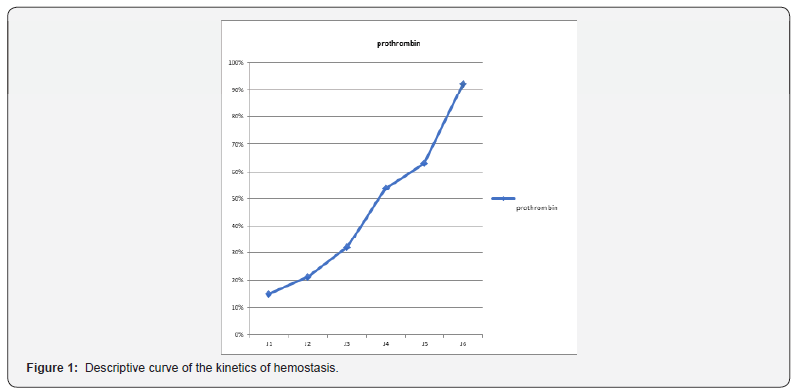
The evolution was quickly favorable. Hyper-bilirubinemia was divided by five in three days, the state of consciousness improved rapidly with appearance of an asterixis, the correction of the hemostasis disorder was more progressive with normalization towards the 4th day (Figure 1), a dramatic improvement in hepatic transaminases was observed as early as the second day (Figure 2). The patient left the intensive care unit to the gastric department on day 6. The symptomatic treatment was continued until day 10, the PBH was performed on day 11 without abnormality then he left the hospital on day 17.
Discussion
IHA is defined as a sudden failure of liver function in a patient with no history of liver disease. The cardinal signs of hepatic failure include coagulopathies and hepatic encephalopathy of any grade in the context of acute liver injury [4]. Currently, there is no scientifically proven beneficial treatment in the treatment of IHC, apart from liver transplantation Lee [5]. More than 1000 drugs have been listed as being responsible of hepatic side effects; 16% of these agents were neuropsychiatric drugs. Antidepressant drugs (tricyclic agents or SSRI), mood stabilizing agents and neuroleptic drugs have been implicated in biological or/and clinical hepatotoxicity. For these reasons, some psychotropic agents have been withdrawn of the pharmaceutical, On the contrary, in case of clinical hepatotoxicity, challenge or maintenance is absolutely inadvisable. Mechanism of the hepatic troubles: precise mechanisms of the hepatotoxicity remain unclear. Contrary to phenothiazine drugs, no information is available on the respective rule of the agents and their metabolites. Hypersensitivity syndrome or eosinophilia has been reported, suggesting a possible immuno-allergic mechanism. Presence of risk factors: risk factors have been retrieved, in some observations, like high daily dosage, high plasmatic concentration, age, alcoholism, obesity or antecedent of hepatic disorders like Gilbert syndrome. [6] Special care is advisable with these patients. As hepatotoxicity has been observed after surd Osage (or suicide attempt), a hepatic check-up has to be performed in these clinical situations [7]. Co-medication with hepatotoxic drugs may increase the risk as it has been suggested. Acetylcysteine is a precursor of glutathione. It is well known as an antidote for acetaminophen overdose due to its ability to increase glutathione levels, which inactivates the toxic metabolite of acetaminophen [8]. N-acetyl-pbenzoquinone mine. Glutathione is a major antioxidant that can serve as a scavenger for free radicals; therefore, acetylcysteine may increase glutathione stock during periods of oxidative stress, increase nitric oxide production, which causes vasodilation and therefore tissue oxygenation, and may also have an antiinflammatory effect. by inhibition of pro-inflammatory factors (TNF alfa and IL8) [9,10]. The majority of studies evaluated the use of NAC in acute IHC secondary to acetaminophen poisoning. There is little research on the use of NAC in IHC secondary to other causes. Hu [8]. evaluated the efficacy of NAC in patients with non-acetaminophen-overdosed IHC (safety and efficacy of NAC in patients with ALF not caused by acetaminophen overdose), in a meta-analysis, which consisted of analyzing four assays prospective clinical trials evaluating NAC versus placebo in the treatment of non-acetaminophen-induced IHC[3].
Conclusion
NAC is a beneficial treatment in the context of nonparacetamol induced IHC, it can prolong the survival of patients with or without liver transplantation and survival after transplantation, but it cannot improve overall survival. Therefore, due to the lack of available scientific evidence, current data is unable to conclusively determine the role of NAC in patients with IHC without paracetamol. Thus, they are unable to make recommendations for clinical practice.
For more open access journal, please click on Juniper Publishers
For more Open Access journal of toxicology articles, please click on Open Access journal of toxicology articles
https://juniperpublishers.com/oajt/OAJT.MS.ID.555638.php

Comments
Post a Comment